Why Pelvic Stretches Matter More Than You Think
Most of us remember to stretch our hamstrings, quads, or shoulders after a workout. But when’s the last time you thought, “Time to stretch my pelvic floor”? Almost never.
And yet, the pelvic floor—the hammock-like web of muscles and connective tissue at the base of your core—does far more than most people realize. It supports posture, mobility, bladder and bowel control, sexual health, and even efficient breathing. When these muscles become too tight, weak, or imbalanced, the effects ripple through daily life: back pain, hip stiffness, urinary leakage, or a constant sense of “locked” tension.
The good news? Recent research (2023–2025) shows that gentle stretching, paired with strengthening and coordination training, can restore balance, improve circulation, and relieve discomfort. Better still, pelvic stretches don’t just support you during workouts—they help during every sit, sneeze, laugh, and step.
In this guide, you’ll discover why pelvic stretches matter more than you think, the best evidence-backed exercises to try, and step-by-step instructions to do them safely and effectively.
What Are the Pelvic Muscles, and Why Stretch Them?
Your pelvic floor is not just one muscle, but a team effort: the levator ani group, coccygeus, fascia, and support ligaments spanning pubic bone to tailbone. Working with the deep core system (transverse abdominis, diaphragm, multifidus), this network:
- Supports the bladder, bowel, uterus/prostate
- Maintains continence
- Provides dynamic stability to hips and spine
- Supports sexual function and sensation
- Adapts to pressure changes (lifting, sneezing, coughing)
Like other muscles, the pelvic floor can be:
- Hypertonic (too tight/overactive): linked to pain, difficulty relaxing, and even worsened symptoms if doing Kegels in isolation.
- Hypotonic (too weak/underactive): tied to leakage, prolapse, or instability.
Stretching addresses relaxation and length. Strengthening develops contractile support. Most people need both, as tension and weakness often coexist.
New Research Updates (2023–2025): Pelvic Health at a Glance
- High prevalence, low care-seeking. Estimates of pelvic floor dysfunction (PFD) range from ~2% to nearly 47% in women; yet only 29% of those with urinary incontinence seek help.
- Widespread symptoms. A 2024 Origin Pelvic Health Study found 83% of women reported at least one pelvic symptom in the past year—yet 96% had not received a diagnosis.
- Aging link. Sarcopenia (muscle wasting) has been connected to incontinence in older women, signaling the pelvic floor’s status as a muscle system vulnerable to age-related decline.
- Exercise works. Trials confirm that pelvic floor muscle training (PFMT)—ideally supervised, 3×/week—improves continence, quality of life, and symptom severity. Stretching builds the “relax” side of this equation.
Benefits of Pelvic Floor Stretching and Relaxation
Stretching your pelvic floor isn’t just about “loosening up.” It offers evidence-backed advantages:
- Reduces hypertonicity & pain. Essential for those with chronic tension, painful intercourse, or pelvic pain syndromes.
- Improves coordination. Relaxation primes the muscles for healthy contraction-relax cycles.
- Supports bladder & bowel function. Encourages relaxation during urination or defecation, making elimination easier and less straining.
- Boosts posture and breathing. A flexible pelvic floor integrates smoothly with the diaphragm for stability.
- Improves quality of life. By lowering leaks, discomfort, and the emotional toll of pelvic dysfunction, stretching contributes to confidence and daily comfort.
The Best Stretching Exercises for Pelvic Muscles
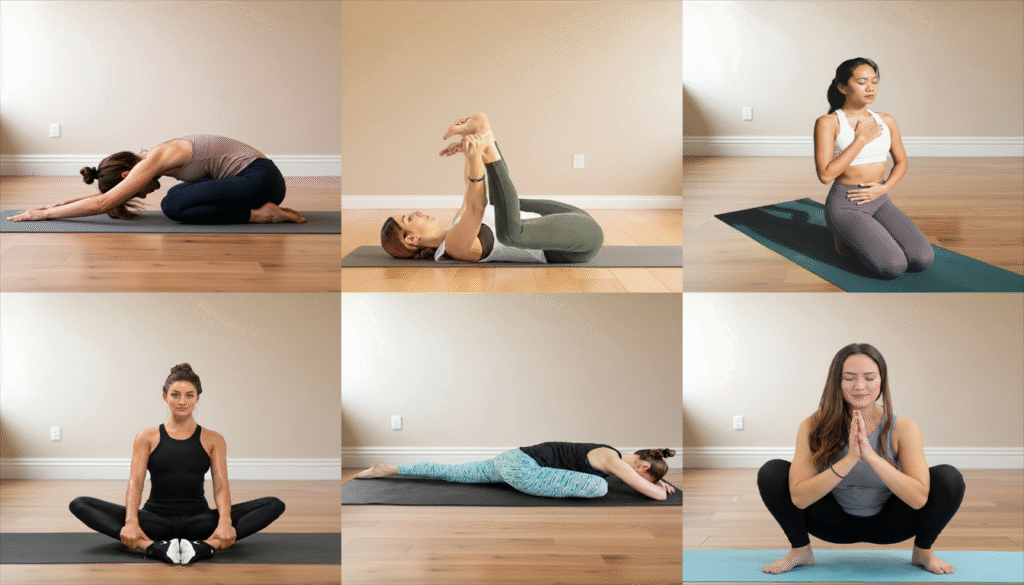
Beginner-Friendly Relaxation Stretches
1. Child’s Pose with Pelvic Sinking

- Kneel, sit back on heels, arms forward, and let the belly soften onto thighs.
- Impact: Gently opens hips and down-regulates pelvic tension.
- Tip: Use a bolster under torso if hips are tight. Breathe into your lower back.
2. Happy Baby Variation

- Lie on your back, bend knees to armpits, hold feet or shins.
- Impact: Releases groin and pelvic muscles.
- Tip: Loop straps around feet for easier access.
3. Supine Diaphragmatic + Balloon Breathing

- On your back, knees bent, hands on lower belly. Inhale, visualizing the pelvic floor dropping open like a balloon; exhale gently and allow recoil.
- Impact: Coordinates breath with pelvic mobility.
Hip-Opening, Pelvic-Soothing Moves
4. Butterfly Stretch

- Sit, soles of feet together, knees wide.
- Impact: Loosens inner thighs and pelvic attachments.
5. Pigeon Pose (Modified)

- Bring one shin across body, extend other leg back.
- Impact: Relieves hip rotator and glute tension, reducing strain on pelvis.
- Tip: Use props to keep upright if needed.
6. Yogi Squat (Malasana)

- Feet wide, squat down, elbows pressing into knees.
- Impact: Deeply opens hips and lengthens pelvic floor.
- Modification: Elevate heels on a blanket if needed.
Combining Stretches With Strength
The “secret sauce” is combining flexibility with strengthening for full-range function.
Sample 10-Minute Flow:
- Diaphragmatic Breathing (2 min)
- Child’s Pose (1 min)
- Happy Baby (1 min)
- Butterfly Stretch (2 min)
- Glute Bridge with pelvic floor engagement (2 min)
- Supine Breathing Reset (2 min)
Case Studies & Clinical Trials (2023–2025)
- Pelvic Yoga vs Conditioning (2024 RCT, n=240): Both groups improved urinary incontinence; pelvic yoga had a modestly higher reduction (~0.3 fewer leaks/day).
- Postpartum Recovery (2025 intervention): Aerobic + resistance + stretching improved pelvic floor contractility and decreased resting tension.
- PFMT Efficacy (2024 Review): Supervised pelvic floor training remains a gold standard for stress urinary incontinence.
- Barriers to Care (2024 qualitative study): Shame, lack of feedback, and uncertainty around “doing it right” prevent adherence—underscoring the value of guided programs.
FAQs:
Q1. How often should I stretch?
Daily, 5–10 minutes is beneficial. With prolapse or extreme laxity, consult a pelvic PT before deep stretches.
Q2. Can men benefit too?
Yes. Men’s pelvic floors support urinary control, sexual function, and core stability. Stretches are equally effective.
Q3. Safe in pregnancy?
Generally yes—with modifications. Stick to gentle, props-supported poses and confirm with your provider.
Q4. Does stretching replace Kegels?
No. Stretching addresses relaxation. Strength (via Kegels or PFMT) addresses support. Both matter.
Q5. When to seek professional help?
Seek a pelvic PT if you experience persistent pain, recurrent leakage, prolapse, or recovery post-surgery.
Final Thoughts: Why Start Pelvic Stretches in 2025
Pelvic health is no longer fringe—it’s mainstream. With studies showing 83% of women experience pelvic-related symptoms yearly (and most undiagnosed), the opportunity for prevention and relief is huge.
Stretching and relaxation act as the “reset button” for pelvic function. But lasting results come from integrated approaches—pairing breathwork, stretching, and strengthening. Think of your pelvic floor as the foundation of a house: resilient, flexible, and responsive enough to carry everything else.
So today, set aside a few minutes for gentle pelvic stretches. Whether you’re recovering postpartum, managing leaks, or simply aiming for better posture, your foundational muscles will thank you with steadier support, freer movement, and more confidence.